
For your body to carry out essential tasks like hormone production, physical activity, and maintaining heart and brain function, it requires energy from food. When food is consumed, it is broken down and nutrients are extracted for specific uses. Carbohydrates are converted into glucose, which enters the bloodstream. In response, the pancreas releases insulin, a hormone that facilitates the movement of glucose into cells for energy, thereby reducing blood sugar levels.
Individuals with diabetes either do not produce enough insulin or are unable to use it effectively to manage blood sugar levels. Consequently, glucose can accumulate in the bloodstream, leaving body cells deprived of energy. Diabetic ketoacidosis (DKA) is a serious complication of diabetes, occurring when cells are so starved of glucose that the body begins breaking down fat stores for energy.
Although this might seem beneficial for weight loss, in DKA, the liver generates excessive ketones, byproducts of fat metabolism. An overabundance of ketones in the bloodstream can render the blood dangerously acidic. If untreated, this pH drop can become toxic, potentially leading to coma or sudden death.
Diabetic ketoacidosis is more common with type 1 diabetes

While type 2 diabetes is more prevalent in the United States and may lead to complications like nerve damage, kidney disease, blood vessel issues, and dementia, type 1 diabetes represents less than 10% of all diabetes cases, according to the U.S. Centers for Disease Control and Prevention. People with type 1 diabetes must take insulin daily to survive, unlike those with type 2 diabetes, who may eventually require insulin. Without a constant insulin supply, type 1 diabetics are at risk for DKA. This condition is rare in type 2 diabetes as they typically produce some insulin, which prevents ketone buildup.
(Read about an insulin pill that may treat type 1 diabetes.)
DKA can occur when a person’s insulin supply is interrupted, whether due to missed injections, insulin pump issues, or incorrect dosing. Illness can also increase DKA risk because controlling blood sugar becomes challenging due to erratic eating and drinking patterns. Other triggers include alcohol or drug use, specific medications, or serious medical events like a heart attack.
Symptoms and prevention of diabetic ketoacidosis
DKA develops over time, making it crucial to recognize early symptoms before they escalate. As blood sugar and ketone levels increase, initial signs include frequent urination and excessive thirst. If not addressed, DKA can result in severe fatigue, difficulty concentrating, dry skin, nausea, shortness of breath, and fruity-smelling breath.
If you have type 1 diabetes and observe these symptoms, the American Diabetes Association advises contacting your doctor or visiting the emergency room. DKA treatment typically involves replenishing lost fluids and electrolytes, and insulin may be administered to stabilize blood sugar levels. If DKA is triggered by an underlying illness or infection, medication to treat that condition may be needed. Notably, taking too much insulin can also be life-threatening.
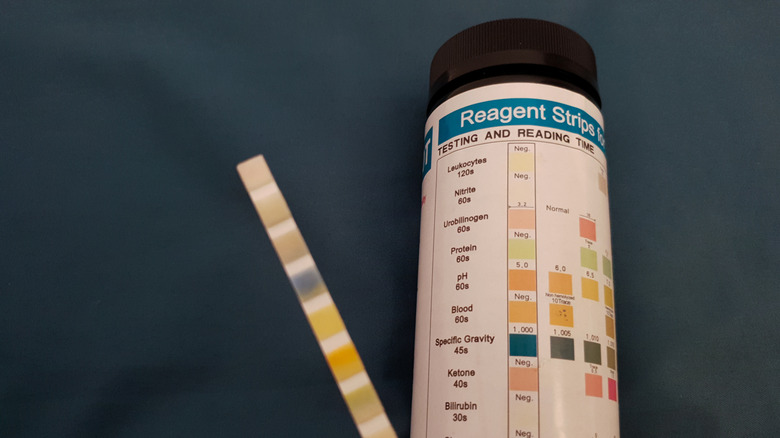
To prevent DKA, diabetics should regularly monitor their blood sugar to ensure it remains within the healthcare team’s target range. If blood sugar levels exceed 240 mg/dL, checking for ketones is advisable, especially if any symptoms are present. Ketone levels can be tested at home using an over-the-counter urine test kit. It’s also crucial to check ketones every few hours when ill, especially if normal eating patterns are disrupted.




